Things to Consider When Modernizing Legacy Systems in Healthcare
- Software
- March 28, 2025
Legacy systems aren’t just inconvenient; they can silently destroy your margins, compliance, and care quality. They may cause your hospital to incur significant costs from data breaches, maintenance, and compromised patient care. This blog serves as a wake-up call, helping you identify whether you have legacy systems in place or not, understand their hidden costs, and explore strategies to modernize systems to achieve better outcomes.
An average day of downtime has the power to cause healthcare entities a loss of $900,000 per day alone. Above that, a cyberattack caused due to loopholes or outdated systems (that is incapable of preventing cyberattacks) can harm your healthcare organization reputation.
NHS (National Health Service) in the UK is the biggest example of it, which became a victim of the WannaCry Ransomware Attack in 2017 due to its outdated legacy system with no up-to-date security patches. NHS faced cancellation of 19,000+ appointments, shutdown of critical systems like MRI scanners, and recovery cost of £92 million + lost productivity. This made them finally invest £150 million to adopt AI for medical imaging and analysis to speed up diagnosis.
Your healthcare organization can face that too for still having legacy systems in place. Hence, we created this blog to help you understand the urgency to modernize your legacy healthcare systems.
What Is a Legacy System in Healthcare?
Legacy systems in healthcare are outdated software or infrastructure that organizations continue to use despite their limitations. These systems were often cutting-edge when first implemented but have become obsolete over time due to technological advancements, changing regulations, and evolving healthcare needs.
Types of healthcare systems that can be modernized:
- Electronic Health Records (EHRs)
- Hospital Information Systems (HIS)
- Practice Management Systems (PMS)
- Laboratory Information Systems (LIS)
- Radiology Information Systems (RIS)
- Picture Archiving and Communication Systems (PACS)
- Pharmacy Management Systems, and more.
Why Healthcare Organizations Still Use Legacy Systems?
The healthcare sector may seem one of the pioneers in embracing the latest tech trends in its innovation yet prefers to stay with its legacy systems because:
- Migrating to new systems can cost millions.
- Transitioning critical systems to modern ones can disrupt patient care as the healthcare sector deals with large-scale data.
- Legacy systems may still meet baseline requirements, like HIPAA.
- Healthcare providers are often resistant to learning new digital systems.
The Hidden Costs of Legacy Healthcare Systems
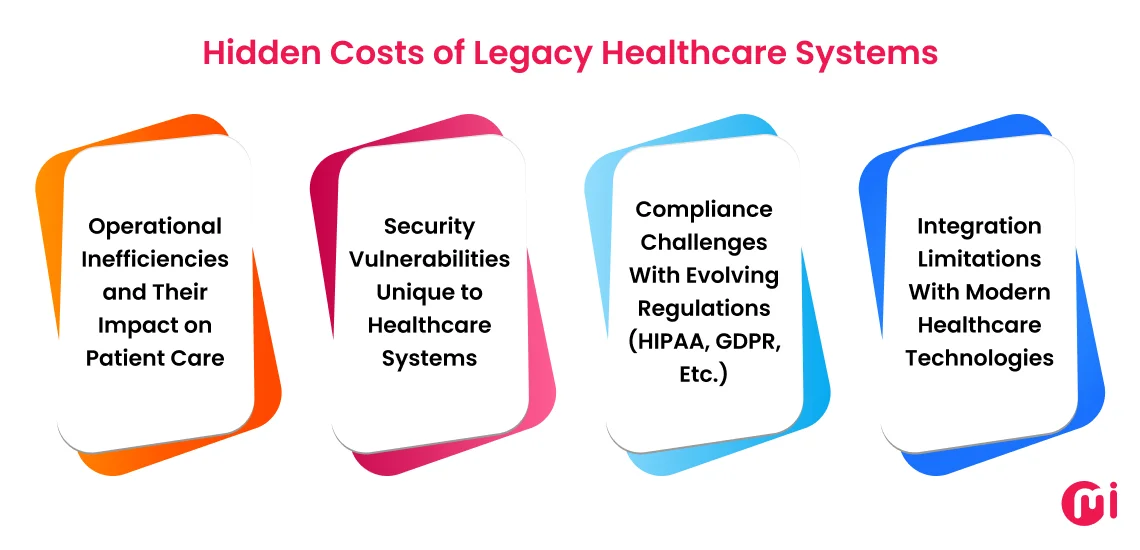
Healthcare organizations should understand that outdated legacy systems may seem convenient, but when seen broadly, they may cost millions of dollars, cripple efficiency, and widen the gap between what healthcare is and what it could be. Below, we have listed a few reasons why you should modernize your legacy healthcare system.
Operational Inefficiencies and Their Impact on Patient Care
Legacy healthcare systems often force clinicians to navigate multiple disconnected interfaces, requiring redundant data entry and creating workflow bottlenecks. Not just that, a siloed healthcare system may cause a significant delay for healthcare providers to receive patient data during emergencies, which may increase mortality risks. Studies show that in emergency healthcare, each hour of delay can lead to a 1% increase in the risk of hospital death.
Security Vulnerabilities Unique to Healthcare Systems
When it comes to valuing the data, healthcare data is worth 10-50X more than financial data. If a healthcare organization still has a legacy system in place, those can be low-hanging fruit for attackers.
Hence, healthcare has always been a favorite target for hackers, specifically for ransomware attacks. If we see the real-world cases, in 2023, the healthcare sector faced 725+ confirmed data attacks reported to OCR with over 133 million records exposed or impermissibly disclosed. On top of that, OCR even reported around a 278% increase in ransomware attacks.
The reason behind this, unlike other industries, healthcare systems often connect to medical devices with their own outdated firmware, creating multiple entry points for attackers.
Compliance Challenges With Evolving Regulations (HIPAA, GDPR, Etc.)
As we know, the healthcare industry is the most lovable target of cyber attackers to get access to sensitive medical data that can earn them millions to billions of dollars. Failing to stop them from exploiting your healthcare systems can cost you a fortune – civil penalties of $137 to over $68,928 per violation + criminal penalties under HIPAA compliance.
Additionally, legacy healthcare systems were built as per that time’s higher configurations. With time, they may find it challenging to meet the evolving demands of healthcare compliance, leading to complex workarounds in legacy systems.
Similarly, accommodating GDPR’s “right to be forgotten” is nearly impossible in many legacy architectures that weren’t built with data deletion capabilities.
Moreover, the information-blocking provisions of the 21st Century Cures Act demand seamless FHIR interoperability, which many healthcare legacy systems lack to facilitate.
Some other compliances may have different requirements, but catering to them all together can be challenging for legacy systems.
Integration Limitations With Modern Healthcare Technologies
As legacy healthcare systems are built with old technology, they may lack API integration capabilities and standardized data formats to integrate flawlessly with modern tech. This also makes it challenging for those systems to integrate smoothly with today’s healthcare software development solutions, including telehealth platforms, remote patient monitoring devices, AI diagnostics, and mobile health applications.
This rigid, monolithic software architecture of legacy healthcare systems becomes an obstacle for healthcare organizations to keep up with today’s tech. These limitations force healthcare organizations to maintain disconnected technology environments, preventing the seamless data flow needed for coordinated care and comprehensive analytics.
Why is it High Time to Modernize Your Legacy Healthcare Systems?
The healthcare industry is racing toward a future defined by AI-driven diagnostics, personalized medicine, and seamless patient experiences. Yet, outdated legacy systems act like anchors, dragging organizations into inefficiency, cyber risk, and much more. Here’s why modernization of legacy systems should be the priority for healthcare organizations:
- Cyberattacks are targeting outdated systems.
- 79% of healthcare organizations globally are using AI in some capacity to improve clinical efficiency, advance research efforts, and aid in precision surgery.
- Siloed data in legacy EHRs slow access to critical patient histories, resulting in delayed diagnostics.
- Manual data entry in legacy systems can cause 10-12% of data entry errors, leading to diagnosis errors.
- Healthcare sector regulators are penalizing legacy healthcare systems that fail to meet modernization standards in terms of security.
- Legacy databases struggle to honor patient data rights, exposing organizations to paying fines of up to 4% of global revenue.
- Legacy systems lack the real-time analytics needed to shift from fee-for-service to value-based models. This can make your healthcare operations a bit inefficient as compared to other organizations that have modernized their healthcare software solutions.
- Normally, enterprise-level hospitals with a global presence process 5,000 claims per month and each manual claim takes 15 minutes, which results in 1,250 staff hours per month. Let’s say, the administrative staff wage is $15 per hour; that means, the hospital is spending nearly $20,000 per month on manual payment processing alone. If they automate these processes by modernizing their legacy systems, they can reduce costs by up to 70%.
The path forward is enterprise application modernization for healthcare institutes. This is not just about keeping up with today’s technology but about future-proofing your organization’s ability to deliver care, comply with regulations, and compete in an AI-driven era.
But the question is, what level or way of modernization does your legacy healthcare software need? The next section resolves that query of yours.

How To Identify That Your Legacy Healthcare System Needs Modernization?
There are many cases in legacy systems that indicate that they need a touch of modernization to stay relevant to today’s tech landscape. Below, we have mentioned some factors, indicating that your legacy healthcare system needs modernization:
System Performance
- Response time degradation beyond acceptable thresholds (more than 50%)
- Unpredictable system crashes occur weekly or more frequently
- The system cannot scale to handle current patient volumes, even after the optimization
Technical Debt
- Programming language is getting outdated
- Vendor no longer provides security updates
- Custom code that’s poorly documented and difficult to maintain
Integration Capability
- Inability to connect with modern healthcare devices and solutions like telehealth or remote monitoring solutions
- Lack of API support or limited API functionality
- Challenges in sharing data with other departments/systems
Data Management
- Inability to support structured and unstructured data types
- Limited data analytics capabilities and even finding it difficult to support quality improvement initiatives or AI integration
- Data silos prevent comprehensive patient insights
- Insufficient ability to handle increasing data volumes
User Experience
- Healthcare providers complaints about workflow inefficiencies
- Increased workarounds being developed by staff
- Training new staff takes 2X longer than the industry standard
- High error rates in data entry or retrieval, like more than 15%.
Compliance & Security
- Systems cannot be configured to meet new regulatory requirements
- It’s challenging to implement modern security protocols
- Audit trails are insufficient for compliance or forensic needs
Cost For Maintenance
- Maintenance cost is increasing more than 15% on a YoY basis
- Support costs exceed 40% of the original system investment
The 9-Step Approach to Strategic Healthcare System Modernization
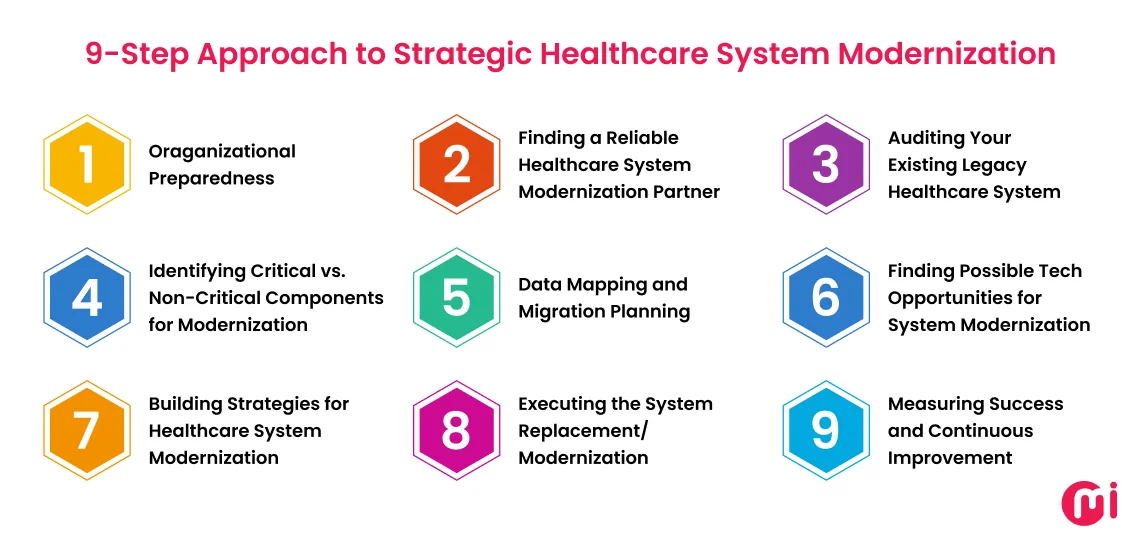
Your healthcare system is a critical part of the administration processes of your facility. Modernizing that legacy system requires the perfect balance between technicals as well as organizational realities. Hence, we created this 9-step framework to modernize your legacy healthcare system, which includes:
STEP 1: Organizational Preparedness
Before a single line of code is rewritten or any system is replaced, healthcare organizations must establish a strong foundation for change. That starts with:
- Understanding stakeholder alignment and organizational readiness in terms of having a decision-making framework to resolve competing priorities.
- Establishing data quality standards, remediation procedures, governance policies to address both technical and institutional practices, and data lifecycle management approaches while adhering to compliance standards.
- Selecting the right approach from phased and complete system replacement to ensure a positive impact on healthcare environments.
- Developing a complete business case for modernization that addresses direct cost savings, clinical and operational efficiency, risk mitigation benefits, and competitive advantages.
- Mapping internal capabilities, identifying resource gaps for external support, developing phased timelines, allocating budget, and establishing contingency reserves for both time and budget.
STEP 2: Finding a Reliable Healthcare System Modernization Partner
In the survey of vFunction, they found 92% of enterprises modernizing their applications (at least one). They also found that four in five respondents (around 79%) admitted the failure of application modernization projects.
One of the many reasons behind this app modernization project’s failure can be the not-so-wise selection of a modernization partner.
Hence, the selection of the right application modernization services provider is necessary, as they can mean the difference between success and costly failure.
For that, you need to set the evaluation criteria, which include factors:
- Technical expertise with both legacy systems and modern healthcare technologies.
- Proven methodology for modernization that addresses healthcare-specific challenges.
- Deep understanding of healthcare workflows and clinical processes.
- Experience with healthcare-specific regulatory requirements, including HIPAA, HITECH, and the 21st Century Cures Act.
- Knowledge of healthcare data standards (HL7, FHIR, DICOM, etc.)
- Familiarity with healthcare-specific integration challenges, including medical devices and specialized clinical systems.
To evaluate the right system modernization partner, you can ask the following questions:
- How have you handled clinical downtime requirements in previous modernization projects?
- What methodology do you use to validate clinical data integrity during migration?
- How do you approach training for clinical staff with limited time availability?
- What contingency planning do you recommend for critical care systems during the transition?
- How have you incorporated emerging technologies like AI while maintaining regulatory compliance?

STEP 3: Auditing Your Existing Legacy Healthcare System
Once you find the right system modernization partner, they can help you do the detailed auditing of existing legacy healthcare systems. This can help to identify even granular areas where modernization can have a considerable impact.
The comprehensive legacy healthcare system audit includes:
- Functionality mapping to document current capabilities and usage patterns
- Technical architecture analysis identifying integration points and dependencies
- Performance benchmarking to establish baselines for improvement measurement
- Security vulnerability assessment highlighting critical risk areas
- Code quality analysis for systems that may be candidates for refactoring rather than replacement
STEP 4: Identifying Critical vs. Non-Critical Components for Modernization
Not all systems require the same level of modernization approach. This requires identifying and bifurcating critical and non-critical components. Your legacy system modernization partner helps to do that with the approach that includes:
- Classifying systems based on patient safety impact and operational necessity.
- Identifying systems with 24/7 availability requirements versus those with acceptable downtime windows.
- Mapping the revenue impact of various components to prioritize financially critical systems.
- Assessing the regulatory implications of different system components.
- Documenting “technical debt hotspots” requiring immediate attention versus areas that can be addressed incrementally.
STEP 5: Data Mapping and Migration Planning
Once the critical and non-critical components of the legacy healthcare system are identified, your healthcare software modernization partner will help you in data mapping and migration planning. The approach for the same may include:
- Opting for a thorough cataloging of all data that exists within your healthcare organization’s IT ecosystem.
- Creating data lineage documentation showing how information flows between systems
- Prioritizing field-level mapping between legacy systems and modernized replacements
- Opting for data quality assessment to identify remediation requirements before migration
- Building an archiving strategy for historical data that balances accessibility with storage costs
STEP 6: Finding Possible Tech Opportunities for System Modernization
There are multiple ways you can modernize your legacy systems. However, finding the best one relevant to today’s tech trends and your industry is a must. Below, we have mentioned tech opportunities you can embrace to improve your healthcare operations:
- AI/ML Integration Possibilities for Specific Healthcare Workflows
- Implementing deep learning and NLP-based clinical decision support solutions to enhance diagnostic accuracy and treatment planning
- Predictive analytics for patient deterioration and readmission risk
- Hospital administrative automation for prior authorizations and claims processing
- Resource optimization for staff scheduling and patient flow
- NLP-based clinical documentation
- Cloud Migration Considerations for Healthcare Environments
- Consider implementing a hybrid cloud for PHI storage (start with non-PHI systems like operational and financial) while ensuring HIPAA-compliant cloud environments with appropriate BAAs.
- Adopt a microservices architecture to break applications into independent services, containerize them for consistency, and use Kubernetes to orchestrate, scale, and manage deployments efficiently.
- Implement cloud-based healthcare data lake architecture for unified analytics.
- Create disaster recovery and business continuity capabilities in cloud environments.
- Interoperability Solutions with Existing Systems
- Adopt API-first architecture to expose legacy functionality to modern applications.
- Ensure FHIR implementation to standardize data exchange across clinical systems.
- Update integration engines to support protocols (both legacy HL7 v2 and modern FHIR/REST interfaces with 99.99% reliability) while maintaining legacy connectivity.
- Implement enterprise service bus implementation to manage complex system interactions.
- Build patient identity management solutions to ensure data integrity across systems.
- Security and Compliance Enhancement Opportunities
- Implement zero-trust models, specifically micro-segmentation solutions that reduce the attack surface by 60-70% with continuous authentication and authorization.
- Deploy AI-powered security monitoring (like UEBA – User and Entity Behavior Analytics) to detect anomalous behavior and potential breaches.
- Leverage compliance automation platforms that reduce audit preparation time by 65% while improving documentation quality.
- Other Emerging Tech Opportunities
- Build a robust virtual care ecosystem integrated with core clinical systems that can help boost provider efficiency by 35% while maintaining 92% patient satisfaction.
- Create a secure Internet of Medical Things (IoMT) infrastructure that can manage 10,000+ connected devices with real-time anomaly detection and 99.999% uptime.
- Implement ambient clinical intelligence solutions for hands-free documentation. This can also help to reduce documentation time by 50% while improving completeness and accuracy.
STEP 7: Building Strategies for Healthcare System Modernization
When building a healthcare application modernization strategy, you should keep 4 key strategies on priority. That includes risk mitigation, phased implementation, staff training & change management, and contingency planning. Below, we tried to cover what’s in all four different strategies for your legacy healthcare system modernization:
Risk Mitigation Planning
- Clinical safety risk assessments for each phase of implementation
- Downtime management planning with clinical workflow alternatives
- Data integrity verification procedures throughout migration
- Regulatory compliance verification at each milestone
- Financial risk management, including cost containment measures
Phased Implementation Approach
- Identify and prioritize “quick win” opportunities to demonstrate value and build momentum
- Plan for sequence implementations that keep up with organizational change capacity
- Balance technical dependencies with organizational priorities
- Establish clear success criteria for each phase before proceeding
- Build feedback loops between phases to incorporate lessons learned
Staff Training and Change Management
- Role-based training programs tailored to different user groups
- Super-user program development to provide peer support during the transition
- Workflow redesign to capture efficiency benefits of new systems
- Metrics to evaluate adoption and identify areas requiring additional support
Contingency Planning for Critical Systems
- Rollback procedures for each implementation phase
- Clinical downtime procedures specific to each affected department
- Technical support escalation paths with clearly defined responsibilities
- Data recovery capabilities for migration issues
- Communication protocols for various contingency scenarios
STEP 8: Executing the System Replacement/Modernization
After careful planning, design, and testing, the next critical phase is executing the replacement or modernization of your legacy healthcare system. This step involves a well-orchestrated rollout that ensures continuity of care, minimizes disruption, and verifies that the new system meets both clinical and regulatory standards. The execution process for this includes:
- Break the modernization into 2-week sprints with clear deliverables (e.g., migrating radiology modules first).
- Hold daily standups with cross-functional teams (IT, clinicians, compliance officers) to address blockers.
- Use containerization (e.g., Docker, Kubernetes) to deploy updates without interrupting live systems.
- Validate HIPAA/GDPR adherence at each milestone (e.g., encryption of migrated patient data).
You can also take the pilot approach that enables you to execute department-based system modernization. Once the pilot is successfully implemented, you can proceed with the full deployment.
Post this, your partner will help to provide comprehensive training sessions for end-users.
STEP 9: Measuring Success and Continuous Improvement
The modernization of your legacy healthcare system doesn’t end with the completion of your full-scale execution. It does require ongoing support and continuous improvements. Below, we have mentioned metrics that you can track to measure the success of your legacy healthcare system modernization and aim for their continuous improvements:
- Technical metrics including uptime, response time, and error rates
- Operational metrics such as task completion time and workflow efficiency
- Financial metrics, including cost per transaction and return on investment
- Clinical metrics focusing on quality and safety improvements
- User satisfaction metrics across different stakeholder groups
How MindInventory Can Be Your Healthcare Legacy System Modernization Companion
Modernizing legacy healthcare systems is a high-stakes journey that demands expertise, precision, and a deep understanding of unique healthcare challenges. At MindInventory, we specialize in transforming outdated systems into agile, AI-driven platforms that empower providers, protect patients, and future-proof operations.
Here’s why you should trust MindInventory for your legacy system modernization project:
- Have been serving global businesses across industries to strategically innovate since 2011.
- Have deep healthcare compliance knowledge (HIPAA, GDPR, HITRUST) and certified cloud partnership – AWS with proven expertise in working with Google Cloud and Microsoft Azure.
- Seamlessly embed AI into legacy workflows.
- Build FHIR/HL7-compliant APIs to unlock data silos for ML training.
- From assessment to post-launch optimization, we handle it all.
- Provide an ROI-driven legacy system modernization roadmap aligned with your healthcare entity-specific goals.
- Embed GDPR/HIPAA safeguards into every layer.
- Cut operational costs by 30-40% with cloud optimization and AI automation.
- Guaranteed 99.999% uptime during cutover with blue-green deployment strategies.
FAQs About Healthcare Software Modernization
Rehosting (lift and shift), refactoring (code optimization), rearchitecting, rebuilding, and replacing are the key strategies for legacy system modernization.
Software maintenance focuses on keeping existing systems functioning through bug fixes, minor updates, and minimal enhancements without changing the fundamental architecture or technology stack.
Software modernization, on the other hand, is a broader transformation that rehosts, refactors, re-platforms, rebuilds, and replaces outdated systems to align with industry-leading technologies, scalability needs, and regulatory standards.
When you opt for legacy system modernization, you may face challenges, such as interoperability issues, data migration, high costs & resource allocation, resistance to change, as well as security & compliance.
Data privacy risks, malware infections, ransomware attacks, insider threats, phishing, and vulnerabilities introduced by new technologies can be the potential security risks you can face during legacy healthcare system modernization.
Modernizing healthcare legacy systems is a complex process, which may take from a few months to a year and more to complete. The timeline for this also depends on factors such as the system’s complexity, the scope of modernization, and the chosen approach.













